
|

 Primary health care is a key focus of the current Canadian health care system, a model that depends on networks of people working together to achieve high quality, empowering, 24 hours a day, 7 days a week, client-focused care. These human networks include all members of the interdisciplinary team including nurses, various work groups and social networks, all centered on or at least referent to the clients of the system, the Canadian public. “Sociology draws attention to health care as a nexus of interlocking institutions, including networks, functions, and structures of health care delivery systems, professions, and public governance as well as organizational and professional structures, institutions and roles” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 238). ICTs are beginning to serve as a critical foundation for making these human networks dynamic and viable.
Primary health care is a key focus of the current Canadian health care system, a model that depends on networks of people working together to achieve high quality, empowering, 24 hours a day, 7 days a week, client-focused care. These human networks include all members of the interdisciplinary team including nurses, various work groups and social networks, all centered on or at least referent to the clients of the system, the Canadian public. “Sociology draws attention to health care as a nexus of interlocking institutions, including networks, functions, and structures of health care delivery systems, professions, and public governance as well as organizational and professional structures, institutions and roles” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 238). ICTs are beginning to serve as a critical foundation for making these human networks dynamic and viable.
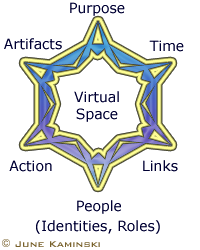
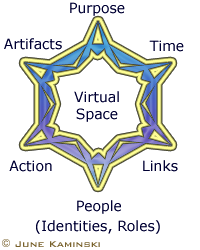
 Networks can perhaps best be viewed through a socio-technical or socio-cultural lens, since social and human-to-human interaction are the key processes involved in any network activity. As well ICTs should also be conceived as socio-technical networks, since they are more than simple tools. “A key idea of social informatics is that information technology is a socio-technical network. ICT in practice is socially shaped. In the highly intertwined model, tech-in-use and a social world are not seen as separate – they co-constitute each other” (Kling, 2000a, p. 248).
Networks can perhaps best be viewed through a socio-technical or socio-cultural lens, since social and human-to-human interaction are the key processes involved in any network activity. As well ICTs should also be conceived as socio-technical networks, since they are more than simple tools. “A key idea of social informatics is that information technology is a socio-technical network. ICT in practice is socially shaped. In the highly intertwined model, tech-in-use and a social world are not seen as separate – they co-constitute each other” (Kling, 2000a, p. 248).
The application of networks in health care requires careful design and awareness of the users of the system. System designers, as well as nurses who serve as guardians and guides of the system need to recognize the life-worlds and work-worlds of the users: in this context, of the health team and the clients they serve. As well, the social context (a matrix of people, service, organization, location, history, and so on) of the ICT use in network activity must be considered since they play “... a significant role in influencing the ways that people use information and technologies” (Kling, 2000a, p. 254).
 Networks within health care can manifest in several different configurations, including client focused networks such as in telenursing, e-health, and client support networks; work related networks including virtual work and virtual social networks; and learning and research networks as in communities of practice. These trends are still in their infancy in most nursing work environments (and personal lives) but they are predicted to be a strong trend in the future. “As the Net generation grows in influence, the trend will be toward networks, not hierarchies, toward open collaboration rather than authority; toward consensus rather than arbitrary edict. The communication support provided by networks and information systems will also alter patterns of social interaction within a health care organization. This technology provides a medium for greater accessibility to shared information and support for rich interpersonal exchange and collaboration across departmental boundaries” (Richards, 2000, p. 10). Networks within health care can manifest in several different configurations, including client focused networks such as in telenursing, e-health, and client support networks; work related networks including virtual work and virtual social networks; and learning and research networks as in communities of practice. These trends are still in their infancy in most nursing work environments (and personal lives) but they are predicted to be a strong trend in the future. “As the Net generation grows in influence, the trend will be toward networks, not hierarchies, toward open collaboration rather than authority; toward consensus rather than arbitrary edict. The communication support provided by networks and information systems will also alter patterns of social interaction within a health care organization. This technology provides a medium for greater accessibility to shared information and support for rich interpersonal exchange and collaboration across departmental boundaries” (Richards, 2000, p. 10).
Virtual Work Networks
 In essence, all organizations consist of networks: systems of people configured into nodes or work teams, occupations, specialties, and hierarchical layers linked by relationships, and all generally focused on a central goal or target. In the case of health care, the central goal is the provision of health care to a network of clients from all walks of life. In recent years, virtual networks within the workplace have become common in many businesses and industries and are a growing phenomena in health care. Seamless work networks require active participation by all of the actors within the health care system, as well as a strong socio-technical infrastructure (Kling, 2000b). The networks intertwine so that “...the technology in use and the social world are not seen as separate, they coconstitute each other (p. 220). In essence, all organizations consist of networks: systems of people configured into nodes or work teams, occupations, specialties, and hierarchical layers linked by relationships, and all generally focused on a central goal or target. In the case of health care, the central goal is the provision of health care to a network of clients from all walks of life. In recent years, virtual networks within the workplace have become common in many businesses and industries and are a growing phenomena in health care. Seamless work networks require active participation by all of the actors within the health care system, as well as a strong socio-technical infrastructure (Kling, 2000b). The networks intertwine so that “...the technology in use and the social world are not seen as separate, they coconstitute each other (p. 220).
 Unfortunately, most current virtual work networks are initiated by administration within health care organizations, usually for the purpose of information dissemination and some employee input. ”Electronic bulletin boards, calendar filings and email enable rapid communication of nursing administrators with staff, nursing managers and support departments (Ball, 2005, p. 2). Although relationships are a core element of a dynamic virtual work network, most Unfortunately, most current virtual work networks are initiated by administration within health care organizations, usually for the purpose of information dissemination and some employee input. ”Electronic bulletin boards, calendar filings and email enable rapid communication of nursing administrators with staff, nursing managers and support departments (Ball, 2005, p. 2). Although relationships are a core element of a dynamic virtual work network, most intranet communication and activity remains top-down and often does not require or expect any response from the recipients. This is logical considering that most health organizations are bureaucratic in nature, where the emphasis is more on order and structure rather than interconnectedness. But trusting relationships are necessary for true virtual networking to occur in the workplace. “Social informatics research investigates intriguing new social phenomena that emerge when people use information technology such as the ways in which people develop trust in virtual teams” (Kling, 2000b, p. 229). Lack of trust in these networks highlight issues of surveillance of communications and network use by administration; confidentiality and privacy issues; and the lack of social support for open two-way or multiple-way interaction. Often a change in leadership and administrative practices are needed: a shift from a bureaucratic model to a more collaborative, equitable mode of interaction across the entire network of players. intranet communication and activity remains top-down and often does not require or expect any response from the recipients. This is logical considering that most health organizations are bureaucratic in nature, where the emphasis is more on order and structure rather than interconnectedness. But trusting relationships are necessary for true virtual networking to occur in the workplace. “Social informatics research investigates intriguing new social phenomena that emerge when people use information technology such as the ways in which people develop trust in virtual teams” (Kling, 2000b, p. 229). Lack of trust in these networks highlight issues of surveillance of communications and network use by administration; confidentiality and privacy issues; and the lack of social support for open two-way or multiple-way interaction. Often a change in leadership and administrative practices are needed: a shift from a bureaucratic model to a more collaborative, equitable mode of interaction across the entire network of players.
Virtual Social Networks
 Virtual social networks are another form of professional network that have expanded phenomenally since the advent of the Internet and other ICTs. “Electronic media do more than just expand access to vast bodies of information. They also serve as a convenient vehicle for building virtual social networks for creating shared knowledge through collaborative learning and problem solving. Cross pollination of ideas through worldwide connectivity can boost creativity synergistically in the co-construction of knowledge” (Bandura, 2002, p. 4). Basically, nursing-related virtual social networks provide a cyberspace for nurses to make contacts, share information and ideas, and build a sense of community. Social technologies are used to provide a dynamic virtual environment, and often provide communicative capabilities through posting tools like blogs, forums, and wikis; email for sharing ideas on a smaller scale; collaborative areas for interaction, Virtual social networks are another form of professional network that have expanded phenomenally since the advent of the Internet and other ICTs. “Electronic media do more than just expand access to vast bodies of information. They also serve as a convenient vehicle for building virtual social networks for creating shared knowledge through collaborative learning and problem solving. Cross pollination of ideas through worldwide connectivity can boost creativity synergistically in the co-construction of knowledge” (Bandura, 2002, p. 4). Basically, nursing-related virtual social networks provide a cyberspace for nurses to make contacts, share information and ideas, and build a sense of community. Social technologies are used to provide a dynamic virtual environment, and often provide communicative capabilities through posting tools like blogs, forums, and wikis; email for sharing ideas on a smaller scale; collaborative areas for interaction, creating and building digital artefacts or planning projects; navigation tools for moving through the virtual network landscape; and profiles to provide a space for each member to disclose personal information with others. Nurses who have to engage in shift-work often find that virtual social networks can provide a sense of connection with other professionals that is available around the clock. Since time is often a factor in any social interchange, virtual communication often offers an alternative for practicing nurses who can access information and interchange at any time of day. With active participation, the interchanges and shared information/ideas of the network can culminate into valuable social and cultural capital, available to all members. Often, nursing virtual social networks are created for the purpose of exchanging ideas on practice issues and best practices; to become more knowledgeable about new trends, research, and innovations in health care; or to participate in advocacy, activist, and educational initiatives. creating and building digital artefacts or planning projects; navigation tools for moving through the virtual network landscape; and profiles to provide a space for each member to disclose personal information with others. Nurses who have to engage in shift-work often find that virtual social networks can provide a sense of connection with other professionals that is available around the clock. Since time is often a factor in any social interchange, virtual communication often offers an alternative for practicing nurses who can access information and interchange at any time of day. With active participation, the interchanges and shared information/ideas of the network can culminate into valuable social and cultural capital, available to all members. Often, nursing virtual social networks are created for the purpose of exchanging ideas on practice issues and best practices; to become more knowledgeable about new trends, research, and innovations in health care; or to participate in advocacy, activist, and educational initiatives.
 Of course, nurses must have both technological and social access to reap any benefits from virtual social networks. Technological access includes actual available ICT equipment including “...computers of adequate speed and equipped with appropriate software for a given activity” (Kling, 1998, p.1) which serve as technologies of interaction within the network context. Social access “...refers to know-how, a mix of professional knowledge, economic resources, and technical skills, to use technologies in ways that enhance professional practices and social life” (p.1) and support the development of complex social network relationships with peers within a virtual landscape. Time and life commitments are also important considerations, since participation in virtual social networks does require that time be applied to the process, a commodity that is often at a premium in a nurse's life. “Expert knowledge sharing includes both proactive and reactive processes. Receiving information on an ongoing basis requires proactively participating in listservs, which requires effective time management for e-mail” (Johnson, 2004, p. 16). Of course, nurses must have both technological and social access to reap any benefits from virtual social networks. Technological access includes actual available ICT equipment including “...computers of adequate speed and equipped with appropriate software for a given activity” (Kling, 1998, p.1) which serve as technologies of interaction within the network context. Social access “...refers to know-how, a mix of professional knowledge, economic resources, and technical skills, to use technologies in ways that enhance professional practices and social life” (p.1) and support the development of complex social network relationships with peers within a virtual landscape. Time and life commitments are also important considerations, since participation in virtual social networks does require that time be applied to the process, a commodity that is often at a premium in a nurse's life. “Expert knowledge sharing includes both proactive and reactive processes. Receiving information on an ongoing basis requires proactively participating in listservs, which requires effective time management for e-mail” (Johnson, 2004, p. 16).
 Lamb and Kling (2002) described a multidimensional view of professional participants in virtual social networks that distinguished them as social actors with four central characteristics: affiliations, environments, interactions and identities. Affiliations referred to dynamic, multi-level, multi-valent, and multi-network social actor relationships shaped by networks of organizational affiliations. Environments were also dynamic and were contingent on ICT quality and pliability. Interactions referred to actions taken to communicate in legitimate ways, with ICTs included as part of the interaction process. As well, people perform socially embedded (role-based), highly specified actions within the network. Finally, identities focused on social actor identities that had an ICT use component and manifested as multi-level identities in the virtual environment. Social actors use ICTS to construct identities and to control perceptions in others. Sawhney and Lee (2000) described how social actors who create unique virtual social networks using ICTs interact with and “discover the new liberties of action of an emerging communication technology” (p.1) and together with other social actors create a space for people to shape a network focused on a common subject or affiliation. Similar technologies are becoming commonly used in the actual provision of nursing care, in the form of telenursing and e-health networks. Lamb and Kling (2002) described a multidimensional view of professional participants in virtual social networks that distinguished them as social actors with four central characteristics: affiliations, environments, interactions and identities. Affiliations referred to dynamic, multi-level, multi-valent, and multi-network social actor relationships shaped by networks of organizational affiliations. Environments were also dynamic and were contingent on ICT quality and pliability. Interactions referred to actions taken to communicate in legitimate ways, with ICTs included as part of the interaction process. As well, people perform socially embedded (role-based), highly specified actions within the network. Finally, identities focused on social actor identities that had an ICT use component and manifested as multi-level identities in the virtual environment. Social actors use ICTS to construct identities and to control perceptions in others. Sawhney and Lee (2000) described how social actors who create unique virtual social networks using ICTs interact with and “discover the new liberties of action of an emerging communication technology” (p.1) and together with other social actors create a space for people to shape a network focused on a common subject or affiliation. Similar technologies are becoming commonly used in the actual provision of nursing care, in the form of telenursing and e-health networks.
Telenursing Networks
 Telenursing is the branch of telehealth that involves actual nursing and client interaction through the medium of information technology. Before the advent of computers, similar activity sometimes occurred using telephones (which still occurs, i.e. the BC NurseLine) or even two-way radio. “Telehealth is the provision of health care or health information using telecommunications technology to provide care or information over long or short distances. It may include consultation, assessment, diagnosis, treatment, transfer of health data, client education and professional development. Telehealth may use familiar technology such as telephone, e-mail, or personal digital assistants, or more complex technology such as remote control surgical instrumentation” (CRNBC, 2005, p. 1). Telenursing is the branch of telehealth that involves actual nursing and client interaction through the medium of information technology. Before the advent of computers, similar activity sometimes occurred using telephones (which still occurs, i.e. the BC NurseLine) or even two-way radio. “Telehealth is the provision of health care or health information using telecommunications technology to provide care or information over long or short distances. It may include consultation, assessment, diagnosis, treatment, transfer of health data, client education and professional development. Telehealth may use familiar technology such as telephone, e-mail, or personal digital assistants, or more complex technology such as remote control surgical instrumentation” (CRNBC, 2005, p. 1).
 Telenursing first evolved to provide expert service to people living in remote areas, but it is becoming more common in urban regions as well. New technologies have added a visual component to the interactions that augments the historic audio exchange. Nurses can actually view healing wounds, can access physiological monitoring equipment to measure physical indicators such as vital signs and provide routine assessment and follow-up care without the client having to travel to the health care agency for an appointment. “Telehealth, considered the use of home-monitoring systems by nurses, may be designed to provide home healthcare nursing services to monitor chronic diseases, such as diabetes. A video monitoring system may be used in conjunction with the monitoring devices at both ends of the system, permitting video and voice interaction between nurse and patient and adding a personal touch” (Moody, 2005, p. 157). Telenursing first evolved to provide expert service to people living in remote areas, but it is becoming more common in urban regions as well. New technologies have added a visual component to the interactions that augments the historic audio exchange. Nurses can actually view healing wounds, can access physiological monitoring equipment to measure physical indicators such as vital signs and provide routine assessment and follow-up care without the client having to travel to the health care agency for an appointment. “Telehealth, considered the use of home-monitoring systems by nurses, may be designed to provide home healthcare nursing services to monitor chronic diseases, such as diabetes. A video monitoring system may be used in conjunction with the monitoring devices at both ends of the system, permitting video and voice interaction between nurse and patient and adding a personal touch” (Moody, 2005, p. 157).
A decidedly modernist approach is often used in the literature to promote and discuss the benefits of telenursing, especially by organizational leadership researchers,  but also by governing nursing organizations such as the College of Registered Nurses of British Columbia (CRNBC). “Telehealth is innovative and rapidly changing to provide more information, quicker communication and instant access within health care. Nurses' in all practice settings can use telehealth to deliver care, provide education, monitor clients' progress, access client records, obtain information and foster communication and collaboration among themselves, other health professionals and clients. Telehealth can be used to replace or complement some components of face-to-face health care. It has the potential to increase accessibility, particularly for clients in rural, remote, or under-served locations. Telehealth may be used to provide more timely, effective and efficient care, and enable the client to remain closer to home. Nurses use telehealth when it can enhance, augment, or otherwise improve care and services for clients” (CRNBC, 2005, p. 1). but also by governing nursing organizations such as the College of Registered Nurses of British Columbia (CRNBC). “Telehealth is innovative and rapidly changing to provide more information, quicker communication and instant access within health care. Nurses' in all practice settings can use telehealth to deliver care, provide education, monitor clients' progress, access client records, obtain information and foster communication and collaboration among themselves, other health professionals and clients. Telehealth can be used to replace or complement some components of face-to-face health care. It has the potential to increase accessibility, particularly for clients in rural, remote, or under-served locations. Telehealth may be used to provide more timely, effective and efficient care, and enable the client to remain closer to home. Nurses use telehealth when it can enhance, augment, or otherwise improve care and services for clients” (CRNBC, 2005, p. 1).
 It does seem logical that some clients would find value in telenursing services, especially if the alternative would require repetitive travel, expense, or isolation from home and significant others. However, nurses need to be aware of the less visible potential effects of providing nursing care “...on screen, instead of behind the screens” (Sandelowski, 2002, p. 64). Nurses need to question if the absence of physical presence and shared physical space detracts from caring and establishing reciprocity with clients. “Nurses have an interest in determining how tele-technologies can be used to maximize health benefits and to enhance the felt presence of the nurse, It does seem logical that some clients would find value in telenursing services, especially if the alternative would require repetitive travel, expense, or isolation from home and significant others. However, nurses need to be aware of the less visible potential effects of providing nursing care “...on screen, instead of behind the screens” (Sandelowski, 2002, p. 64). Nurses need to question if the absence of physical presence and shared physical space detracts from caring and establishing reciprocity with clients. “Nurses have an interest in determining how tele-technologies can be used to maximize health benefits and to enhance the felt presence of the nurse,  but they also have an interest in understanding how these technologies can undermine the presence of the nurse. Tele-health practices not only call for nurses to reconceptualize presence, place, and bodies in nursing, but also to explore how these practices threaten to displace nursing” (p. 65). There is a danger that both nurses and clients can enter a sort of shadow land as they dissolve into the virtual interface. It is imperative for any nurse who engages in telenursing to be aware of this, and to ensure that network exchanges with their clients reflect dynamic, personable caring and attentiveness, even when the interactions occur via ICT mediums. In telenursing, it is the nurse who is responsible and accountable for ensuring that the client is never perceived as a “ ...hypertexted, hyperreal representation on screen in the form of a rhythm strip; black-and-white or colorized image; or numeric, graphic, digital, schematic, or other visual display” (p. 66). but they also have an interest in understanding how these technologies can undermine the presence of the nurse. Tele-health practices not only call for nurses to reconceptualize presence, place, and bodies in nursing, but also to explore how these practices threaten to displace nursing” (p. 65). There is a danger that both nurses and clients can enter a sort of shadow land as they dissolve into the virtual interface. It is imperative for any nurse who engages in telenursing to be aware of this, and to ensure that network exchanges with their clients reflect dynamic, personable caring and attentiveness, even when the interactions occur via ICT mediums. In telenursing, it is the nurse who is responsible and accountable for ensuring that the client is never perceived as a “ ...hypertexted, hyperreal representation on screen in the form of a rhythm strip; black-and-white or colorized image; or numeric, graphic, digital, schematic, or other visual display” (p. 66).
 It is theoretically possible, if the technology used is sophisticated enough to provide clear, crisp visuals, real-time relay, exceptional audio, and accurate physiological measurement, that an astute and technologically literate nurse could create a similar sense of caring, presence, and individualized attention with the client, using telenursing ICTs. Still, virtual environments for nursing care could challenge the nurse's ability to perceive the digitalized presentation of the client as an individual, and provide individualized care. “For nurses especially, they trouble the distinction between human being/body and information network, and between body work and information work. Yet they offer nurses an opportunity to move toward an informatics of the body and a more embodied informatics in nursing; that is, toward an orientation to nursing education, practice, and research that celebrates the body work of nursing and reunites it with the information work of nursing” (Sandelowski, 2002, p. 67). It is theoretically possible, if the technology used is sophisticated enough to provide clear, crisp visuals, real-time relay, exceptional audio, and accurate physiological measurement, that an astute and technologically literate nurse could create a similar sense of caring, presence, and individualized attention with the client, using telenursing ICTs. Still, virtual environments for nursing care could challenge the nurse's ability to perceive the digitalized presentation of the client as an individual, and provide individualized care. “For nurses especially, they trouble the distinction between human being/body and information network, and between body work and information work. Yet they offer nurses an opportunity to move toward an informatics of the body and a more embodied informatics in nursing; that is, toward an orientation to nursing education, practice, and research that celebrates the body work of nursing and reunites it with the information work of nursing” (Sandelowski, 2002, p. 67).
 While engaging with the virtual representation of a client, the nurse must strive to envision and experience the client's three dimensional body and being in order to accurately advise, assess, diagnose, and interact fully and dynamically. This perceiving must occur within the a virtual network environment, where both body-sense and body-awareness are combined with digital information. “Nurses must see body and information work as constituting each other, and the body as a source of knowledge and power for nursing. Because nurses occupy a distinctive place in the health care arena, they have a distinctive contribution to make to theorizing the body in the virtual environments of care now emerging” (Sandelowski, 2002, p. 68). Not only the body, but also the person's inner being must be acknowledged and somehow included. While engaging with the virtual representation of a client, the nurse must strive to envision and experience the client's three dimensional body and being in order to accurately advise, assess, diagnose, and interact fully and dynamically. This perceiving must occur within the a virtual network environment, where both body-sense and body-awareness are combined with digital information. “Nurses must see body and information work as constituting each other, and the body as a source of knowledge and power for nursing. Because nurses occupy a distinctive place in the health care arena, they have a distinctive contribution to make to theorizing the body in the virtual environments of care now emerging” (Sandelowski, 2002, p. 68). Not only the body, but also the person's inner being must be acknowledged and somehow included.
 What are the psychological and emotional effects of being examined and assessed via a video camera? Is the sense of intimacy and privacy common in caring client-nurse interchanges lost in the virtual translation? These are questions that nurses must consider before engaging in telenursing network interactions and activities. The ideal scenario would be that nurses and ICT designers could work together to create more sophisticated ICTs that could meet the needs of the clients better. “Although they seem far removed from each other, both media designers and nurses share a common interest in presence: in how to create it, how to use it effectively, and how it works to generate its effects. At the heart of all efforts to enhance media is the creation of the illusion that technologically mediated experiences, such as tele-health encounters and virtual reality, are not mediated at all; that is, to create the perception of presence. The design intentions behind distance technologies are to overcome the effects of distance and electronic mediation; that is, to simulate lifelike and full-bodied encounters in proximate space that close the distance between people and allow users to feel as if they were,...reaching out to touch someone” (Sandelowski, 2002, p. 65). What are the psychological and emotional effects of being examined and assessed via a video camera? Is the sense of intimacy and privacy common in caring client-nurse interchanges lost in the virtual translation? These are questions that nurses must consider before engaging in telenursing network interactions and activities. The ideal scenario would be that nurses and ICT designers could work together to create more sophisticated ICTs that could meet the needs of the clients better. “Although they seem far removed from each other, both media designers and nurses share a common interest in presence: in how to create it, how to use it effectively, and how it works to generate its effects. At the heart of all efforts to enhance media is the creation of the illusion that technologically mediated experiences, such as tele-health encounters and virtual reality, are not mediated at all; that is, to create the perception of presence. The design intentions behind distance technologies are to overcome the effects of distance and electronic mediation; that is, to simulate lifelike and full-bodied encounters in proximate space that close the distance between people and allow users to feel as if they were,...reaching out to touch someone” (Sandelowski, 2002, p. 65).
E-health Networks
 Another critically important wave of network evolvement is the public use of the Internet for networking with health care providers and other members of the public, now called E-health. Essentially, E-health is a client-centered World Wide Web-based network where clients and health care providers collaborate through ICT mediums to research, seek, manage, deliver, refer, arrange, and consult with others about health related information and concerns (Moody, 2005; Conte, 1999). “The spread of powerful computers among a large and rapidly increasing segment of the population, and their interconnection through the Internet and millions of powerful servers, has brought an entirely new and largely unexpected quality to health and health informatics, and is effecting changes that we are only beginning to fathom. Essentially, it provided a vehicle to tie the general population in a new way into the system of health provision, health maintenance and health care. According to many assessments, health care is among the foremost reasons for resorting to the Internet” (Moehr & Grant, 2000, p. 278). Another critically important wave of network evolvement is the public use of the Internet for networking with health care providers and other members of the public, now called E-health. Essentially, E-health is a client-centered World Wide Web-based network where clients and health care providers collaborate through ICT mediums to research, seek, manage, deliver, refer, arrange, and consult with others about health related information and concerns (Moody, 2005; Conte, 1999). “The spread of powerful computers among a large and rapidly increasing segment of the population, and their interconnection through the Internet and millions of powerful servers, has brought an entirely new and largely unexpected quality to health and health informatics, and is effecting changes that we are only beginning to fathom. Essentially, it provided a vehicle to tie the general population in a new way into the system of health provision, health maintenance and health care. According to many assessments, health care is among the foremost reasons for resorting to the Internet” (Moehr & Grant, 2000, p. 278).
 Although E-health developed from the telehealth network movement, it is a unique phenomena in two ways: networks and resources devoted to E-health have developed on the Internet at an amazing rate over the past decade or so, and the emphasis is genuinely client focused. “It differs from telehealth or telemedicine in that e-health is Internet-based and includes a range of services, nursing or healthcare, health education, and medication prescription or refills via e-prescribing. In conjunction, telemonitoring devices may be used, via a Universal Serial Bus (USB) port on the patient's computer, to collect additional physiologic data (e.g blood pressure, pulse, temperature, weight, spirometry, blood glucose, and oxygen saturation levels)” (Moody, 2005, p. 157). Although E-health developed from the telehealth network movement, it is a unique phenomena in two ways: networks and resources devoted to E-health have developed on the Internet at an amazing rate over the past decade or so, and the emphasis is genuinely client focused. “It differs from telehealth or telemedicine in that e-health is Internet-based and includes a range of services, nursing or healthcare, health education, and medication prescription or refills via e-prescribing. In conjunction, telemonitoring devices may be used, via a Universal Serial Bus (USB) port on the patient's computer, to collect additional physiologic data (e.g blood pressure, pulse, temperature, weight, spirometry, blood glucose, and oxygen saturation levels)” (Moody, 2005, p. 157).
 The phenomenal growth of E-health can not generally be credited to the health care system or its employed social actors. Rather, clients driven by the need and urge to become informed health consumers and participants have catalyzed this new style of networking, clients who have learned to utilize ICTs in the form of the Internet to meet their health concern needs. Although statistics show that women are underrepresented in Internet usage, women tend to access the Internet more than men to seek health related information and networking (Henwood, Wyatt, Hart & Smith, 2003). “The notion of informed choice is inductive of the greater agency and sense of empowerment said to be experienced by such patients. The dominant discourse here is said to be one of rights, where patients have the right to information and are treated as individuals, not treatment opportunities” (p. 591). The phenomenal growth of E-health can not generally be credited to the health care system or its employed social actors. Rather, clients driven by the need and urge to become informed health consumers and participants have catalyzed this new style of networking, clients who have learned to utilize ICTs in the form of the Internet to meet their health concern needs. Although statistics show that women are underrepresented in Internet usage, women tend to access the Internet more than men to seek health related information and networking (Henwood, Wyatt, Hart & Smith, 2003). “The notion of informed choice is inductive of the greater agency and sense of empowerment said to be experienced by such patients. The dominant discourse here is said to be one of rights, where patients have the right to information and are treated as individuals, not treatment opportunities” (p. 591).
 Informed, reflective clients in the health care system have encountered some degree of alarm and reluctance from members of the health team, since the notion requires a change in the dynamics of provider-patient or provider-client interactions. “It is clear that the informed patient will not emerge naturally or easily within existing structures and relationships. Constraints exist within both practitioner and patient communities and within the Informed, reflective clients in the health care system have encountered some degree of alarm and reluctance from members of the health team, since the notion requires a change in the dynamics of provider-patient or provider-client interactions. “It is clear that the informed patient will not emerge naturally or easily within existing structures and relationships. Constraints exist within both practitioner and patient communities and within the space occupied by both in the medical encounter” (Henwood et al, 2003, p. 605). E-health networks that support interactions between knowledgeable clients who have assumed a position of control and choice in their own health care and reciprocal health professionals depend upon a shift in perspective on the part of health care providers, especially in medicine and nursing. A health care landscape that is conducive to a partnership level of interaction is critical, while the onus of control rests with the client (Moehr & Grant, 2000). “These trends are also leading informatics, as an information-intensive industry, to become a major pillar of health care. Because the person is the only element in common across institutional, organizational, and national boundaries, we come full circle, to the need to re-design systems around the person, that is, to patient centered informatics. IT facilitates the transmission of health care information without regard to location; it contributes to the trend toward boundary-less delivery of both health information and health care” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 240). space occupied by both in the medical encounter” (Henwood et al, 2003, p. 605). E-health networks that support interactions between knowledgeable clients who have assumed a position of control and choice in their own health care and reciprocal health professionals depend upon a shift in perspective on the part of health care providers, especially in medicine and nursing. A health care landscape that is conducive to a partnership level of interaction is critical, while the onus of control rests with the client (Moehr & Grant, 2000). “These trends are also leading informatics, as an information-intensive industry, to become a major pillar of health care. Because the person is the only element in common across institutional, organizational, and national boundaries, we come full circle, to the need to re-design systems around the person, that is, to patient centered informatics. IT facilitates the transmission of health care information without regard to location; it contributes to the trend toward boundary-less delivery of both health information and health care” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 240).
 Nurses can be primary actors in the virtual arena of E-health, serving as health advisors, Internet guides to help clients select reliable information resources, support group liaisons, web information providers, and so on. Nurses need to be involved in the design and implementation of E-health portals and programs that provide the best possible E-health experience for health care clients. Designers of such programs should be directed to “...build tools to enable individuals to become involved in their cure no matter where they are. Such tools may include programs for monitoring one's own health and health behaviours, tools for accessing quality information, and tools for communicating with others in like circumstances or with health professionals” (Kaplan et al, 2001, p. 239). Nurses can be primary actors in the virtual arena of E-health, serving as health advisors, Internet guides to help clients select reliable information resources, support group liaisons, web information providers, and so on. Nurses need to be involved in the design and implementation of E-health portals and programs that provide the best possible E-health experience for health care clients. Designers of such programs should be directed to “...build tools to enable individuals to become involved in their cure no matter where they are. Such tools may include programs for monitoring one's own health and health behaviours, tools for accessing quality information, and tools for communicating with others in like circumstances or with health professionals” (Kaplan et al, 2001, p. 239).
 It is becoming obvious, that many clients want health care that is “highly personalized, customized, targeted, with tailored information and ultimately care delivery and case management” (Kaplan & Flatley Brennan, 2001, p. 311). This has led to the evolution of many client managed E-health initiatives that serve as self-help or support group networks. Initiators of these networks embrace the role of significant provider as well as user of health information, providing advice and a virtual environment that invites interaction with others who are focused on the same health issues and questions (Henwood et al, 2003). The levels of affiliation and interaction that develops within some of these networks are truly inspirational to health care providers who wish to engage in E-health networks with clients. Nurses can become visible social agents within these networks, interacting with informed, reflective public agents who have the desire and capabilities to make the health care choices that suit their own life world and personal values. It is becoming obvious, that many clients want health care that is “highly personalized, customized, targeted, with tailored information and ultimately care delivery and case management” (Kaplan & Flatley Brennan, 2001, p. 311). This has led to the evolution of many client managed E-health initiatives that serve as self-help or support group networks. Initiators of these networks embrace the role of significant provider as well as user of health information, providing advice and a virtual environment that invites interaction with others who are focused on the same health issues and questions (Henwood et al, 2003). The levels of affiliation and interaction that develops within some of these networks are truly inspirational to health care providers who wish to engage in E-health networks with clients. Nurses can become visible social agents within these networks, interacting with informed, reflective public agents who have the desire and capabilities to make the health care choices that suit their own life world and personal values.
Communities of Practice
 Communities of Practice (COP) are another example of professional networks that can interact using ICTs including the Internet to collaborate on a variety of projects or initiatives, often for the sake of research or education (which are sometimes called Communities of Learning or learning communties). These networks can be viewed through the lens of social cognitive theory to reveal the enactment of collective agency. “People's shared belief in their combined power to achieve desired results is a key ingredient of collective agency. Perceived collective efficiency raises people's vision of what they wish to achieve, enhances motivational commitment to their missions, strengthens resilience to adversity, and enhances performance accomplishments” (Bandura, 2002, p. 3). Communities of Practice (COP) are another example of professional networks that can interact using ICTs including the Internet to collaborate on a variety of projects or initiatives, often for the sake of research or education (which are sometimes called Communities of Learning or learning communties). These networks can be viewed through the lens of social cognitive theory to reveal the enactment of collective agency. “People's shared belief in their combined power to achieve desired results is a key ingredient of collective agency. Perceived collective efficiency raises people's vision of what they wish to achieve, enhances motivational commitment to their missions, strengthens resilience to adversity, and enhances performance accomplishments” (Bandura, 2002, p. 3).
Shortliffe, Barnett, Cimino, Greenes, Huff, and Patel described the Intermed project, which served as a model for informatics-related COP networking, which depended on Internet-based ICTs as a virtual meeting space for the community. Collectively, the social agents of this incubated “...the idea of an electronically mediated, research collaboration, a collaboratory. A national collaboratory is a center without walls, in which the nation's researchers can perform their research without regard to geographic location – interacting with colleagues, accessing instrumentation, sharing data, and computational resources and accessing information in digital libraries. The Intermed project seeks to demonstrate the viability of the collaboratory concept in the context of medical informatics research” ( 1996, p. 1).
 Although COPs are relatively new in nursing, the literature does support the benefits of such intiatives, by describing the value to nursing through “...the “doing” of community within the context of shared projects, obligations, and goals” (Page & Scott, 2001, p. 528). In fact, COPs are acknowledged as a prime vehicle for achieving the goal of informatics integration into nursing education. “Creative faculty development strategies that capitalize on the concept of faculty as a community of practice are required to incorporate informatics competencies into nursing curricula” (Barton, 2005, p. 323). Although COPs are usually devoted to rather formal, critical issues and foci, there is a tendency to also encourage open, creative thinking and affective interaction within the socio-technical arena. “We develop the concept of “learning communities” to meet the need for democratic, inclusive, and on-going innovation ... We conceptualize 'learning communities” as dialogic and “playful” spaces within which members can draw creatively on their differences while constructing shared knowledge” (Page & Scott, 2001, p. 528). The virtual social space of COPs ideally invites collaborative inquiry, a sharing of learning or research goals as well as process, within a holistic, action-oriented network. Although COPs are relatively new in nursing, the literature does support the benefits of such intiatives, by describing the value to nursing through “...the “doing” of community within the context of shared projects, obligations, and goals” (Page & Scott, 2001, p. 528). In fact, COPs are acknowledged as a prime vehicle for achieving the goal of informatics integration into nursing education. “Creative faculty development strategies that capitalize on the concept of faculty as a community of practice are required to incorporate informatics competencies into nursing curricula” (Barton, 2005, p. 323). Although COPs are usually devoted to rather formal, critical issues and foci, there is a tendency to also encourage open, creative thinking and affective interaction within the socio-technical arena. “We develop the concept of “learning communities” to meet the need for democratic, inclusive, and on-going innovation ... We conceptualize 'learning communities” as dialogic and “playful” spaces within which members can draw creatively on their differences while constructing shared knowledge” (Page & Scott, 2001, p. 528). The virtual social space of COPs ideally invites collaborative inquiry, a sharing of learning or research goals as well as process, within a holistic, action-oriented network.
 Wenger, McDermott and Snyder (2002) identified seven key principles for COP cultivation: design for evolution, open a dialogue between inside and outside perspectives, invite different levels of participation, develop both public and private community spaces, focus on value, combine familiarity and excitement, and create a rhythm for the community. Wenger also identified four general categories of COP, all of which fit well within nursing ideals and intents: helping communities, best-practice communities, knowledge-stewarding communities, and innovation communities. COP need to be actively created and sustained, which requires well developed relational links and abilities between the social actors, both human and technical. Wenger, McDermott and Snyder (2002) identified seven key principles for COP cultivation: design for evolution, open a dialogue between inside and outside perspectives, invite different levels of participation, develop both public and private community spaces, focus on value, combine familiarity and excitement, and create a rhythm for the community. Wenger also identified four general categories of COP, all of which fit well within nursing ideals and intents: helping communities, best-practice communities, knowledge-stewarding communities, and innovation communities. COP need to be actively created and sustained, which requires well developed relational links and abilities between the social actors, both human and technical.
 The issues of inclusion/exclusion and social access (or the lack thereof) are potential critical consequences of any health oriented network. Clients and health professionals alike could be disadvantaged if other modes of interaction are not available. “The information society might be conceptualized as a powerful technoeconomic network that is creating a new social reality. Drawing on the work of Latour, Star has described the way heterogeneous interests can be pulled together into 'mini-empires' enrolling both human and non-human actors into new techno-social networks. Once stabilized, these networks begin to shape our social landscape, grounding each and every social action and movement. Within these networks, new sets of physical-social conventions are established, which being stable for non-members, also creates new forms of marginality” (Page & Scott, 2001, p. 549). The issues of inclusion/exclusion and social access (or the lack thereof) are potential critical consequences of any health oriented network. Clients and health professionals alike could be disadvantaged if other modes of interaction are not available. “The information society might be conceptualized as a powerful technoeconomic network that is creating a new social reality. Drawing on the work of Latour, Star has described the way heterogeneous interests can be pulled together into 'mini-empires' enrolling both human and non-human actors into new techno-social networks. Once stabilized, these networks begin to shape our social landscape, grounding each and every social action and movement. Within these networks, new sets of physical-social conventions are established, which being stable for non-members, also creates new forms of marginality” (Page & Scott, 2001, p. 549).
|

|




 Primary health care is a key focus of the current Canadian health care system, a model that depends on networks of people working together to achieve high quality, empowering, 24 hours a day, 7 days a week, client-focused care. These human networks include all members of the interdisciplinary team including nurses, various work groups and social networks, all centered on or at least referent to the clients of the system, the Canadian public. “Sociology draws attention to health care as a nexus of interlocking institutions, including networks, functions, and structures of health care delivery systems, professions, and public governance as well as organizational and professional structures, institutions and roles” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 238). ICTs are beginning to serve as a critical foundation for making these human networks dynamic and viable.
Primary health care is a key focus of the current Canadian health care system, a model that depends on networks of people working together to achieve high quality, empowering, 24 hours a day, 7 days a week, client-focused care. These human networks include all members of the interdisciplinary team including nurses, various work groups and social networks, all centered on or at least referent to the clients of the system, the Canadian public. “Sociology draws attention to health care as a nexus of interlocking institutions, including networks, functions, and structures of health care delivery systems, professions, and public governance as well as organizational and professional structures, institutions and roles” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 238). ICTs are beginning to serve as a critical foundation for making these human networks dynamic and viable.  Networks can perhaps best be viewed through a socio-technical or socio-cultural lens, since social and human-to-human interaction are the key processes involved in any network activity. As well ICTs should also be conceived as socio-technical networks, since they are more than simple tools. “A key idea of social informatics is that information technology is a socio-technical network. ICT in practice is socially shaped. In the highly intertwined model, tech-in-use and a social world are not seen as separate – they co-constitute each other” (Kling, 2000a, p. 248).
Networks can perhaps best be viewed through a socio-technical or socio-cultural lens, since social and human-to-human interaction are the key processes involved in any network activity. As well ICTs should also be conceived as socio-technical networks, since they are more than simple tools. “A key idea of social informatics is that information technology is a socio-technical network. ICT in practice is socially shaped. In the highly intertwined model, tech-in-use and a social world are not seen as separate – they co-constitute each other” (Kling, 2000a, p. 248).  Networks within health care can manifest in several different configurations, including client focused networks such as in telenursing, e-health, and client support networks; work related networks including virtual work and virtual social networks; and learning and research networks as in communities of practice. These trends are still in their infancy in most nursing work environments (and personal lives) but they are predicted to be a strong trend in the future. “As the Net generation grows in influence, the trend will be toward networks, not hierarchies, toward open collaboration rather than authority; toward consensus rather than arbitrary edict. The communication support provided by networks and information systems will also alter patterns of social interaction within a health care organization. This technology provides a medium for greater accessibility to shared information and support for rich interpersonal exchange and collaboration across departmental boundaries” (Richards, 2000, p. 10).
Networks within health care can manifest in several different configurations, including client focused networks such as in telenursing, e-health, and client support networks; work related networks including virtual work and virtual social networks; and learning and research networks as in communities of practice. These trends are still in their infancy in most nursing work environments (and personal lives) but they are predicted to be a strong trend in the future. “As the Net generation grows in influence, the trend will be toward networks, not hierarchies, toward open collaboration rather than authority; toward consensus rather than arbitrary edict. The communication support provided by networks and information systems will also alter patterns of social interaction within a health care organization. This technology provides a medium for greater accessibility to shared information and support for rich interpersonal exchange and collaboration across departmental boundaries” (Richards, 2000, p. 10).
 In essence, all organizations consist of networks: systems of people configured into nodes or work teams, occupations, specialties, and hierarchical layers linked by relationships, and all generally focused on a central goal or target. In the case of health care, the central goal is the provision of health care to a network of clients from all walks of life. In recent years, virtual networks within the workplace have become common in many businesses and industries and are a growing phenomena in health care. Seamless work networks require active participation by all of the actors within the health care system, as well as a strong socio-technical infrastructure (Kling, 2000b). The networks intertwine so that “...the technology in use and the social world are not seen as separate, they coconstitute each other (p. 220).
In essence, all organizations consist of networks: systems of people configured into nodes or work teams, occupations, specialties, and hierarchical layers linked by relationships, and all generally focused on a central goal or target. In the case of health care, the central goal is the provision of health care to a network of clients from all walks of life. In recent years, virtual networks within the workplace have become common in many businesses and industries and are a growing phenomena in health care. Seamless work networks require active participation by all of the actors within the health care system, as well as a strong socio-technical infrastructure (Kling, 2000b). The networks intertwine so that “...the technology in use and the social world are not seen as separate, they coconstitute each other (p. 220).  Unfortunately, most current virtual work networks are initiated by administration within health care organizations, usually for the purpose of information dissemination and some employee input. ”Electronic bulletin boards, calendar filings and email enable rapid communication of nursing administrators with staff, nursing managers and support departments (Ball, 2005, p. 2). Although relationships are a core element of a dynamic virtual work network, most
Unfortunately, most current virtual work networks are initiated by administration within health care organizations, usually for the purpose of information dissemination and some employee input. ”Electronic bulletin boards, calendar filings and email enable rapid communication of nursing administrators with staff, nursing managers and support departments (Ball, 2005, p. 2). Although relationships are a core element of a dynamic virtual work network, most intranet communication and activity remains top-down and often does not require or expect any response from the recipients. This is logical considering that most health organizations are bureaucratic in nature, where the emphasis is more on order and structure rather than interconnectedness. But trusting relationships are necessary for true virtual networking to occur in the workplace. “Social informatics research investigates intriguing new social phenomena that emerge when people use information technology such as the ways in which people develop trust in virtual teams” (Kling, 2000b, p. 229). Lack of trust in these networks highlight issues of surveillance of communications and network use by administration; confidentiality and privacy issues; and the lack of social support for open two-way or multiple-way interaction. Often a change in leadership and administrative practices are needed: a shift from a bureaucratic model to a more collaborative, equitable mode of interaction across the entire network of players.
intranet communication and activity remains top-down and often does not require or expect any response from the recipients. This is logical considering that most health organizations are bureaucratic in nature, where the emphasis is more on order and structure rather than interconnectedness. But trusting relationships are necessary for true virtual networking to occur in the workplace. “Social informatics research investigates intriguing new social phenomena that emerge when people use information technology such as the ways in which people develop trust in virtual teams” (Kling, 2000b, p. 229). Lack of trust in these networks highlight issues of surveillance of communications and network use by administration; confidentiality and privacy issues; and the lack of social support for open two-way or multiple-way interaction. Often a change in leadership and administrative practices are needed: a shift from a bureaucratic model to a more collaborative, equitable mode of interaction across the entire network of players.
 Virtual social networks are another form of professional network that have expanded phenomenally since the advent of the Internet and other ICTs. “Electronic media do more than just expand access to vast bodies of information. They also serve as a convenient vehicle for building virtual social networks for creating shared knowledge through collaborative learning and problem solving. Cross pollination of ideas through worldwide connectivity can boost creativity synergistically in the co-construction of knowledge” (Bandura, 2002, p. 4). Basically, nursing-related virtual social networks provide a cyberspace for nurses to make contacts, share information and ideas, and build a sense of community. Social technologies are used to provide a dynamic virtual environment, and often provide communicative capabilities through posting tools like blogs, forums, and wikis; email for sharing ideas on a smaller scale; collaborative areas for interaction,
Virtual social networks are another form of professional network that have expanded phenomenally since the advent of the Internet and other ICTs. “Electronic media do more than just expand access to vast bodies of information. They also serve as a convenient vehicle for building virtual social networks for creating shared knowledge through collaborative learning and problem solving. Cross pollination of ideas through worldwide connectivity can boost creativity synergistically in the co-construction of knowledge” (Bandura, 2002, p. 4). Basically, nursing-related virtual social networks provide a cyberspace for nurses to make contacts, share information and ideas, and build a sense of community. Social technologies are used to provide a dynamic virtual environment, and often provide communicative capabilities through posting tools like blogs, forums, and wikis; email for sharing ideas on a smaller scale; collaborative areas for interaction, creating and building digital artefacts or planning projects; navigation tools for moving through the virtual network landscape; and profiles to provide a space for each member to disclose personal information with others. Nurses who have to engage in shift-work often find that virtual social networks can provide a sense of connection with other professionals that is available around the clock. Since time is often a factor in any social interchange, virtual communication often offers an alternative for practicing nurses who can access information and interchange at any time of day. With active participation, the interchanges and shared information/ideas of the network can culminate into valuable social and cultural capital, available to all members. Often, nursing virtual social networks are created for the purpose of exchanging ideas on practice issues and best practices; to become more knowledgeable about new trends, research, and innovations in health care; or to participate in advocacy, activist, and educational initiatives.
creating and building digital artefacts or planning projects; navigation tools for moving through the virtual network landscape; and profiles to provide a space for each member to disclose personal information with others. Nurses who have to engage in shift-work often find that virtual social networks can provide a sense of connection with other professionals that is available around the clock. Since time is often a factor in any social interchange, virtual communication often offers an alternative for practicing nurses who can access information and interchange at any time of day. With active participation, the interchanges and shared information/ideas of the network can culminate into valuable social and cultural capital, available to all members. Often, nursing virtual social networks are created for the purpose of exchanging ideas on practice issues and best practices; to become more knowledgeable about new trends, research, and innovations in health care; or to participate in advocacy, activist, and educational initiatives.
 Of course, nurses must have both technological and social access to reap any benefits from virtual social networks. Technological access includes actual available ICT equipment including “...computers of adequate speed and equipped with appropriate software for a given activity” (Kling, 1998, p.1) which serve as technologies of interaction within the network context. Social access “...refers to know-how, a mix of professional knowledge, economic resources, and technical skills, to use technologies in ways that enhance professional practices and social life” (p.1) and support the development of complex social network relationships with peers within a virtual landscape. Time and life commitments are also important considerations, since participation in virtual social networks does require that time be applied to the process, a commodity that is often at a premium in a nurse's life. “Expert knowledge sharing includes both proactive and reactive processes. Receiving information on an ongoing basis requires proactively participating in listservs, which requires effective time management for e-mail” (Johnson, 2004, p. 16).
Of course, nurses must have both technological and social access to reap any benefits from virtual social networks. Technological access includes actual available ICT equipment including “...computers of adequate speed and equipped with appropriate software for a given activity” (Kling, 1998, p.1) which serve as technologies of interaction within the network context. Social access “...refers to know-how, a mix of professional knowledge, economic resources, and technical skills, to use technologies in ways that enhance professional practices and social life” (p.1) and support the development of complex social network relationships with peers within a virtual landscape. Time and life commitments are also important considerations, since participation in virtual social networks does require that time be applied to the process, a commodity that is often at a premium in a nurse's life. “Expert knowledge sharing includes both proactive and reactive processes. Receiving information on an ongoing basis requires proactively participating in listservs, which requires effective time management for e-mail” (Johnson, 2004, p. 16).  Lamb and Kling (2002) described a multidimensional view of professional participants in virtual social networks that distinguished them as social actors with four central characteristics: affiliations, environments, interactions and identities. Affiliations referred to dynamic, multi-level, multi-valent, and multi-network social actor relationships shaped by networks of organizational affiliations. Environments were also dynamic and were contingent on ICT quality and pliability. Interactions referred to actions taken to communicate in legitimate ways, with ICTs included as part of the interaction process. As well, people perform socially embedded (role-based), highly specified actions within the network. Finally, identities focused on social actor identities that had an ICT use component and manifested as multi-level identities in the virtual environment. Social actors use ICTS to construct identities and to control perceptions in others. Sawhney and Lee (2000) described how social actors who create unique virtual social networks using ICTs interact with and “discover the new liberties of action of an emerging communication technology” (p.1) and together with other social actors create a space for people to shape a network focused on a common subject or affiliation. Similar technologies are becoming commonly used in the actual provision of nursing care, in the form of telenursing and e-health networks.
Lamb and Kling (2002) described a multidimensional view of professional participants in virtual social networks that distinguished them as social actors with four central characteristics: affiliations, environments, interactions and identities. Affiliations referred to dynamic, multi-level, multi-valent, and multi-network social actor relationships shaped by networks of organizational affiliations. Environments were also dynamic and were contingent on ICT quality and pliability. Interactions referred to actions taken to communicate in legitimate ways, with ICTs included as part of the interaction process. As well, people perform socially embedded (role-based), highly specified actions within the network. Finally, identities focused on social actor identities that had an ICT use component and manifested as multi-level identities in the virtual environment. Social actors use ICTS to construct identities and to control perceptions in others. Sawhney and Lee (2000) described how social actors who create unique virtual social networks using ICTs interact with and “discover the new liberties of action of an emerging communication technology” (p.1) and together with other social actors create a space for people to shape a network focused on a common subject or affiliation. Similar technologies are becoming commonly used in the actual provision of nursing care, in the form of telenursing and e-health networks.
 Telenursing is the branch of telehealth that involves actual nursing and client interaction through the medium of information technology. Before the advent of computers, similar activity sometimes occurred using telephones (which still occurs, i.e. the BC NurseLine) or even two-way radio. “Telehealth is the provision of health care or health information using telecommunications technology to provide care or information over long or short distances. It may include consultation, assessment, diagnosis, treatment, transfer of health data, client education and professional development. Telehealth may use familiar technology such as telephone, e-mail, or personal digital assistants, or more complex technology such as remote control surgical instrumentation” (CRNBC, 2005, p. 1).
Telenursing is the branch of telehealth that involves actual nursing and client interaction through the medium of information technology. Before the advent of computers, similar activity sometimes occurred using telephones (which still occurs, i.e. the BC NurseLine) or even two-way radio. “Telehealth is the provision of health care or health information using telecommunications technology to provide care or information over long or short distances. It may include consultation, assessment, diagnosis, treatment, transfer of health data, client education and professional development. Telehealth may use familiar technology such as telephone, e-mail, or personal digital assistants, or more complex technology such as remote control surgical instrumentation” (CRNBC, 2005, p. 1).  Telenursing first evolved to provide expert service to people living in remote areas, but it is becoming more common in urban regions as well. New technologies have added a visual component to the interactions that augments the historic audio exchange. Nurses can actually view healing wounds, can access physiological monitoring equipment to measure physical indicators such as vital signs and provide routine assessment and follow-up care without the client having to travel to the health care agency for an appointment. “Telehealth, considered the use of home-monitoring systems by nurses, may be designed to provide home healthcare nursing services to monitor chronic diseases, such as diabetes. A video monitoring system may be used in conjunction with the monitoring devices at both ends of the system, permitting video and voice interaction between nurse and patient and adding a personal touch” (Moody, 2005, p. 157).
Telenursing first evolved to provide expert service to people living in remote areas, but it is becoming more common in urban regions as well. New technologies have added a visual component to the interactions that augments the historic audio exchange. Nurses can actually view healing wounds, can access physiological monitoring equipment to measure physical indicators such as vital signs and provide routine assessment and follow-up care without the client having to travel to the health care agency for an appointment. “Telehealth, considered the use of home-monitoring systems by nurses, may be designed to provide home healthcare nursing services to monitor chronic diseases, such as diabetes. A video monitoring system may be used in conjunction with the monitoring devices at both ends of the system, permitting video and voice interaction between nurse and patient and adding a personal touch” (Moody, 2005, p. 157). but also by governing nursing organizations such as the College of Registered Nurses of British Columbia (CRNBC). “Telehealth is innovative and rapidly changing to provide more information, quicker communication and instant access within health care. Nurses' in all practice settings can use telehealth to deliver care, provide education, monitor clients' progress, access client records, obtain information and foster communication and collaboration among themselves, other health professionals and clients. Telehealth can be used to replace or complement some components of face-to-face health care. It has the potential to increase accessibility, particularly for clients in rural, remote, or under-served locations. Telehealth may be used to provide more timely, effective and efficient care, and enable the client to remain closer to home. Nurses use telehealth when it can enhance, augment, or otherwise improve care and services for clients” (CRNBC, 2005, p. 1).
but also by governing nursing organizations such as the College of Registered Nurses of British Columbia (CRNBC). “Telehealth is innovative and rapidly changing to provide more information, quicker communication and instant access within health care. Nurses' in all practice settings can use telehealth to deliver care, provide education, monitor clients' progress, access client records, obtain information and foster communication and collaboration among themselves, other health professionals and clients. Telehealth can be used to replace or complement some components of face-to-face health care. It has the potential to increase accessibility, particularly for clients in rural, remote, or under-served locations. Telehealth may be used to provide more timely, effective and efficient care, and enable the client to remain closer to home. Nurses use telehealth when it can enhance, augment, or otherwise improve care and services for clients” (CRNBC, 2005, p. 1).  It does seem logical that some clients would find value in telenursing services, especially if the alternative would require repetitive travel, expense, or isolation from home and significant others. However, nurses need to be aware of the less visible potential effects of providing nursing care “...on screen, instead of behind the screens” (Sandelowski, 2002, p. 64). Nurses need to question if the absence of physical presence and shared physical space detracts from caring and establishing reciprocity with clients. “Nurses have an interest in determining how tele-technologies can be used to maximize health benefits and to enhance the felt presence of the nurse,
It does seem logical that some clients would find value in telenursing services, especially if the alternative would require repetitive travel, expense, or isolation from home and significant others. However, nurses need to be aware of the less visible potential effects of providing nursing care “...on screen, instead of behind the screens” (Sandelowski, 2002, p. 64). Nurses need to question if the absence of physical presence and shared physical space detracts from caring and establishing reciprocity with clients. “Nurses have an interest in determining how tele-technologies can be used to maximize health benefits and to enhance the felt presence of the nurse,  but they also have an interest in understanding how these technologies can undermine the presence of the nurse. Tele-health practices not only call for nurses to reconceptualize presence, place, and bodies in nursing, but also to explore how these practices threaten to displace nursing” (p. 65). There is a danger that both nurses and clients can enter a sort of shadow land as they dissolve into the virtual interface. It is imperative for any nurse who engages in telenursing to be aware of this, and to ensure that network exchanges with their clients reflect dynamic, personable caring and attentiveness, even when the interactions occur via ICT mediums. In telenursing, it is the nurse who is responsible and accountable for ensuring that the client is never perceived as a “ ...hypertexted, hyperreal representation on screen in the form of a rhythm strip; black-and-white or colorized image; or numeric, graphic, digital, schematic, or other visual display” (p. 66).
but they also have an interest in understanding how these technologies can undermine the presence of the nurse. Tele-health practices not only call for nurses to reconceptualize presence, place, and bodies in nursing, but also to explore how these practices threaten to displace nursing” (p. 65). There is a danger that both nurses and clients can enter a sort of shadow land as they dissolve into the virtual interface. It is imperative for any nurse who engages in telenursing to be aware of this, and to ensure that network exchanges with their clients reflect dynamic, personable caring and attentiveness, even when the interactions occur via ICT mediums. In telenursing, it is the nurse who is responsible and accountable for ensuring that the client is never perceived as a “ ...hypertexted, hyperreal representation on screen in the form of a rhythm strip; black-and-white or colorized image; or numeric, graphic, digital, schematic, or other visual display” (p. 66).  It is theoretically possible, if the technology used is sophisticated enough to provide clear, crisp visuals, real-time relay, exceptional audio, and accurate physiological measurement, that an astute and technologically literate nurse could create a similar sense of caring, presence, and individualized attention with the client, using telenursing ICTs. Still, virtual environments for nursing care could challenge the nurse's ability to perceive the digitalized presentation of the client as an individual, and provide individualized care. “For nurses especially, they trouble the distinction between human being/body and information network, and between body work and information work. Yet they offer nurses an opportunity to move toward an informatics of the body and a more embodied informatics in nursing; that is, toward an orientation to nursing education, practice, and research that celebrates the body work of nursing and reunites it with the information work of nursing” (Sandelowski, 2002, p. 67).
It is theoretically possible, if the technology used is sophisticated enough to provide clear, crisp visuals, real-time relay, exceptional audio, and accurate physiological measurement, that an astute and technologically literate nurse could create a similar sense of caring, presence, and individualized attention with the client, using telenursing ICTs. Still, virtual environments for nursing care could challenge the nurse's ability to perceive the digitalized presentation of the client as an individual, and provide individualized care. “For nurses especially, they trouble the distinction between human being/body and information network, and between body work and information work. Yet they offer nurses an opportunity to move toward an informatics of the body and a more embodied informatics in nursing; that is, toward an orientation to nursing education, practice, and research that celebrates the body work of nursing and reunites it with the information work of nursing” (Sandelowski, 2002, p. 67). While engaging with the virtual representation of a client, the nurse must strive to envision and experience the client's three dimensional body and being in order to accurately advise, assess, diagnose, and interact fully and dynamically. This perceiving must occur within the a virtual network environment, where both body-sense and body-awareness are combined with digital information. “Nurses must see body and information work as constituting each other, and the body as a source of knowledge and power for nursing. Because nurses occupy a distinctive place in the health care arena, they have a distinctive contribution to make to theorizing the body in the virtual environments of care now emerging” (Sandelowski, 2002, p. 68). Not only the body, but also the person's inner being must be acknowledged and somehow included.
While engaging with the virtual representation of a client, the nurse must strive to envision and experience the client's three dimensional body and being in order to accurately advise, assess, diagnose, and interact fully and dynamically. This perceiving must occur within the a virtual network environment, where both body-sense and body-awareness are combined with digital information. “Nurses must see body and information work as constituting each other, and the body as a source of knowledge and power for nursing. Because nurses occupy a distinctive place in the health care arena, they have a distinctive contribution to make to theorizing the body in the virtual environments of care now emerging” (Sandelowski, 2002, p. 68). Not only the body, but also the person's inner being must be acknowledged and somehow included.  What are the psychological and emotional effects of being examined and assessed via a video camera? Is the sense of intimacy and privacy common in caring client-nurse interchanges lost in the virtual translation? These are questions that nurses must consider before engaging in telenursing network interactions and activities. The ideal scenario would be that nurses and ICT designers could work together to create more sophisticated ICTs that could meet the needs of the clients better. “Although they seem far removed from each other, both media designers and nurses share a common interest in presence: in how to create it, how to use it effectively, and how it works to generate its effects. At the heart of all efforts to enhance media is the creation of the illusion that technologically mediated experiences, such as tele-health encounters and virtual reality, are not mediated at all; that is, to create the perception of presence. The design intentions behind distance technologies are to overcome the effects of distance and electronic mediation; that is, to simulate lifelike and full-bodied encounters in proximate space that close the distance between people and allow users to feel as if they were,...reaching out to touch someone” (Sandelowski, 2002, p. 65).
What are the psychological and emotional effects of being examined and assessed via a video camera? Is the sense of intimacy and privacy common in caring client-nurse interchanges lost in the virtual translation? These are questions that nurses must consider before engaging in telenursing network interactions and activities. The ideal scenario would be that nurses and ICT designers could work together to create more sophisticated ICTs that could meet the needs of the clients better. “Although they seem far removed from each other, both media designers and nurses share a common interest in presence: in how to create it, how to use it effectively, and how it works to generate its effects. At the heart of all efforts to enhance media is the creation of the illusion that technologically mediated experiences, such as tele-health encounters and virtual reality, are not mediated at all; that is, to create the perception of presence. The design intentions behind distance technologies are to overcome the effects of distance and electronic mediation; that is, to simulate lifelike and full-bodied encounters in proximate space that close the distance between people and allow users to feel as if they were,...reaching out to touch someone” (Sandelowski, 2002, p. 65).
 Another critically important wave of network evolvement is the public use of the Internet for networking with health care providers and other members of the public, now called E-health. Essentially, E-health is a client-centered World Wide Web-based network where clients and health care providers collaborate through ICT mediums to research, seek, manage, deliver, refer, arrange, and consult with others about health related information and concerns (Moody, 2005; Conte, 1999). “The spread of powerful computers among a large and rapidly increasing segment of the population, and their interconnection through the Internet and millions of powerful servers, has brought an entirely new and largely unexpected quality to health and health informatics, and is effecting changes that we are only beginning to fathom. Essentially, it provided a vehicle to tie the general population in a new way into the system of health provision, health maintenance and health care. According to many assessments, health care is among the foremost reasons for resorting to the Internet” (Moehr & Grant, 2000, p. 278).
Another critically important wave of network evolvement is the public use of the Internet for networking with health care providers and other members of the public, now called E-health. Essentially, E-health is a client-centered World Wide Web-based network where clients and health care providers collaborate through ICT mediums to research, seek, manage, deliver, refer, arrange, and consult with others about health related information and concerns (Moody, 2005; Conte, 1999). “The spread of powerful computers among a large and rapidly increasing segment of the population, and their interconnection through the Internet and millions of powerful servers, has brought an entirely new and largely unexpected quality to health and health informatics, and is effecting changes that we are only beginning to fathom. Essentially, it provided a vehicle to tie the general population in a new way into the system of health provision, health maintenance and health care. According to many assessments, health care is among the foremost reasons for resorting to the Internet” (Moehr & Grant, 2000, p. 278).
 Although E-health developed from the telehealth network movement, it is a unique phenomena in two ways: networks and resources devoted to E-health have developed on the Internet at an amazing rate over the past decade or so, and the emphasis is genuinely client focused. “It differs from telehealth or telemedicine in that e-health is Internet-based and includes a range of services, nursing or healthcare, health education, and medication prescription or refills via e-prescribing. In conjunction, telemonitoring devices may be used, via a Universal Serial Bus (USB) port on the patient's computer, to collect additional physiologic data (e.g blood pressure, pulse, temperature, weight, spirometry, blood glucose, and oxygen saturation levels)” (Moody, 2005, p. 157).
Although E-health developed from the telehealth network movement, it is a unique phenomena in two ways: networks and resources devoted to E-health have developed on the Internet at an amazing rate over the past decade or so, and the emphasis is genuinely client focused. “It differs from telehealth or telemedicine in that e-health is Internet-based and includes a range of services, nursing or healthcare, health education, and medication prescription or refills via e-prescribing. In conjunction, telemonitoring devices may be used, via a Universal Serial Bus (USB) port on the patient's computer, to collect additional physiologic data (e.g blood pressure, pulse, temperature, weight, spirometry, blood glucose, and oxygen saturation levels)” (Moody, 2005, p. 157). The phenomenal growth of E-health can not generally be credited to the health care system or its employed social actors. Rather, clients driven by the need and urge to become informed health consumers and participants have catalyzed this new style of networking, clients who have learned to utilize ICTs in the form of the Internet to meet their health concern needs. Although statistics show that women are underrepresented in Internet usage, women tend to access the Internet more than men to seek health related information and networking (Henwood, Wyatt, Hart & Smith, 2003). “The notion of informed choice is inductive of the greater agency and sense of empowerment said to be experienced by such patients. The dominant discourse here is said to be one of rights, where patients have the right to information and are treated as individuals, not treatment opportunities” (p. 591).
The phenomenal growth of E-health can not generally be credited to the health care system or its employed social actors. Rather, clients driven by the need and urge to become informed health consumers and participants have catalyzed this new style of networking, clients who have learned to utilize ICTs in the form of the Internet to meet their health concern needs. Although statistics show that women are underrepresented in Internet usage, women tend to access the Internet more than men to seek health related information and networking (Henwood, Wyatt, Hart & Smith, 2003). “The notion of informed choice is inductive of the greater agency and sense of empowerment said to be experienced by such patients. The dominant discourse here is said to be one of rights, where patients have the right to information and are treated as individuals, not treatment opportunities” (p. 591).  Informed, reflective clients in the health care system have encountered some degree of alarm and reluctance from members of the health team, since the notion requires a change in the dynamics of provider-patient or provider-client interactions. “It is clear that the informed patient will not emerge naturally or easily within existing structures and relationships. Constraints exist within both practitioner and patient communities and within the
Informed, reflective clients in the health care system have encountered some degree of alarm and reluctance from members of the health team, since the notion requires a change in the dynamics of provider-patient or provider-client interactions. “It is clear that the informed patient will not emerge naturally or easily within existing structures and relationships. Constraints exist within both practitioner and patient communities and within the space occupied by both in the medical encounter” (Henwood et al, 2003, p. 605). E-health networks that support interactions between knowledgeable clients who have assumed a position of control and choice in their own health care and reciprocal health professionals depend upon a shift in perspective on the part of health care providers, especially in medicine and nursing. A health care landscape that is conducive to a partnership level of interaction is critical, while the onus of control rests with the client (Moehr & Grant, 2000). “These trends are also leading informatics, as an information-intensive industry, to become a major pillar of health care. Because the person is the only element in common across institutional, organizational, and national boundaries, we come full circle, to the need to re-design systems around the person, that is, to patient centered informatics. IT facilitates the transmission of health care information without regard to location; it contributes to the trend toward boundary-less delivery of both health information and health care” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 240).
space occupied by both in the medical encounter” (Henwood et al, 2003, p. 605). E-health networks that support interactions between knowledgeable clients who have assumed a position of control and choice in their own health care and reciprocal health professionals depend upon a shift in perspective on the part of health care providers, especially in medicine and nursing. A health care landscape that is conducive to a partnership level of interaction is critical, while the onus of control rests with the client (Moehr & Grant, 2000). “These trends are also leading informatics, as an information-intensive industry, to become a major pillar of health care. Because the person is the only element in common across institutional, organizational, and national boundaries, we come full circle, to the need to re-design systems around the person, that is, to patient centered informatics. IT facilitates the transmission of health care information without regard to location; it contributes to the trend toward boundary-less delivery of both health information and health care” (Kaplan, Flatley-Brennan, Dowling, Friedman & Peel, 2001, p. 240). Nurses can be primary actors in the virtual arena of E-health, serving as health advisors, Internet guides to help clients select reliable information resources, support group liaisons, web information providers, and so on. Nurses need to be involved in the design and implementation of E-health portals and programs that provide the best possible E-health experience for health care clients. Designers of such programs should be directed to “...build tools to enable individuals to become involved in their cure no matter where they are. Such tools may include programs for monitoring one's own health and health behaviours, tools for accessing quality information, and tools for communicating with others in like circumstances or with health professionals” (Kaplan et al, 2001, p. 239).
Nurses can be primary actors in the virtual arena of E-health, serving as health advisors, Internet guides to help clients select reliable information resources, support group liaisons, web information providers, and so on. Nurses need to be involved in the design and implementation of E-health portals and programs that provide the best possible E-health experience for health care clients. Designers of such programs should be directed to “...build tools to enable individuals to become involved in their cure no matter where they are. Such tools may include programs for monitoring one's own health and health behaviours, tools for accessing quality information, and tools for communicating with others in like circumstances or with health professionals” (Kaplan et al, 2001, p. 239). It is becoming obvious, that many clients want health care that is “highly personalized, customized, targeted, with tailored information and ultimately care delivery and case management” (Kaplan & Flatley Brennan, 2001, p. 311). This has led to the evolution of many client managed E-health initiatives that serve as self-help or support group networks. Initiators of these networks embrace the role of significant provider as well as user of health information, providing advice and a virtual environment that invites interaction with others who are focused on the same health issues and questions (Henwood et al, 2003). The levels of affiliation and interaction that develops within some of these networks are truly inspirational to health care providers who wish to engage in E-health networks with clients. Nurses can become visible social agents within these networks, interacting with informed, reflective public agents who have the desire and capabilities to make the health care choices that suit their own life world and personal values.
It is becoming obvious, that many clients want health care that is “highly personalized, customized, targeted, with tailored information and ultimately care delivery and case management” (Kaplan & Flatley Brennan, 2001, p. 311). This has led to the evolution of many client managed E-health initiatives that serve as self-help or support group networks. Initiators of these networks embrace the role of significant provider as well as user of health information, providing advice and a virtual environment that invites interaction with others who are focused on the same health issues and questions (Henwood et al, 2003). The levels of affiliation and interaction that develops within some of these networks are truly inspirational to health care providers who wish to engage in E-health networks with clients. Nurses can become visible social agents within these networks, interacting with informed, reflective public agents who have the desire and capabilities to make the health care choices that suit their own life world and personal values.
 Communities of Practice (COP) are another example of professional networks that can interact using ICTs including the Internet to collaborate on a variety of projects or initiatives, often for the sake of research or education (which are sometimes called Communities of Learning or learning communties). These networks can be viewed through the lens of social cognitive theory to reveal the enactment of collective agency. “People's shared belief in their combined power to achieve desired results is a key ingredient of collective agency. Perceived collective efficiency raises people's vision of what they wish to achieve, enhances motivational commitment to their missions, strengthens resilience to adversity, and enhances performance accomplishments” (Bandura, 2002, p. 3).
Communities of Practice (COP) are another example of professional networks that can interact using ICTs including the Internet to collaborate on a variety of projects or initiatives, often for the sake of research or education (which are sometimes called Communities of Learning or learning communties). These networks can be viewed through the lens of social cognitive theory to reveal the enactment of collective agency. “People's shared belief in their combined power to achieve desired results is a key ingredient of collective agency. Perceived collective efficiency raises people's vision of what they wish to achieve, enhances motivational commitment to their missions, strengthens resilience to adversity, and enhances performance accomplishments” (Bandura, 2002, p. 3).  Although COPs are relatively new in nursing, the literature does support the benefits of such intiatives, by describing the value to nursing through “...the “doing” of community within the context of shared projects, obligations, and goals” (Page & Scott, 2001, p. 528). In fact, COPs are acknowledged as a prime vehicle for achieving the goal of informatics integration into nursing education. “Creative faculty development strategies that capitalize on the concept of faculty as a community of practice are required to incorporate informatics competencies into nursing curricula” (Barton, 2005, p. 323). Although COPs are usually devoted to rather formal, critical issues and foci, there is a tendency to also encourage open, creative thinking and affective interaction within the socio-technical arena. “We develop the concept of “learning communities” to meet the need for democratic, inclusive, and on-going innovation ... We conceptualize 'learning communities” as dialogic and “playful” spaces within which members can draw creatively on their differences while constructing shared knowledge” (Page & Scott, 2001, p. 528). The virtual social space of COPs ideally invites collaborative inquiry, a sharing of learning or research goals as well as process, within a holistic, action-oriented network.
Although COPs are relatively new in nursing, the literature does support the benefits of such intiatives, by describing the value to nursing through “...the “doing” of community within the context of shared projects, obligations, and goals” (Page & Scott, 2001, p. 528). In fact, COPs are acknowledged as a prime vehicle for achieving the goal of informatics integration into nursing education. “Creative faculty development strategies that capitalize on the concept of faculty as a community of practice are required to incorporate informatics competencies into nursing curricula” (Barton, 2005, p. 323). Although COPs are usually devoted to rather formal, critical issues and foci, there is a tendency to also encourage open, creative thinking and affective interaction within the socio-technical arena. “We develop the concept of “learning communities” to meet the need for democratic, inclusive, and on-going innovation ... We conceptualize 'learning communities” as dialogic and “playful” spaces within which members can draw creatively on their differences while constructing shared knowledge” (Page & Scott, 2001, p. 528). The virtual social space of COPs ideally invites collaborative inquiry, a sharing of learning or research goals as well as process, within a holistic, action-oriented network.  Wenger, McDermott and Snyder (2002) identified seven key principles for COP cultivation: design for evolution, open a dialogue between inside and outside perspectives, invite different levels of participation, develop both public and private community spaces, focus on value, combine familiarity and excitement, and create a rhythm for the community. Wenger also identified four general categories of COP, all of which fit well within nursing ideals and intents: helping communities, best-practice communities, knowledge-stewarding communities, and innovation communities. COP need to be actively created and sustained, which requires well developed relational links and abilities between the social actors, both human and technical.
Wenger, McDermott and Snyder (2002) identified seven key principles for COP cultivation: design for evolution, open a dialogue between inside and outside perspectives, invite different levels of participation, develop both public and private community spaces, focus on value, combine familiarity and excitement, and create a rhythm for the community. Wenger also identified four general categories of COP, all of which fit well within nursing ideals and intents: helping communities, best-practice communities, knowledge-stewarding communities, and innovation communities. COP need to be actively created and sustained, which requires well developed relational links and abilities between the social actors, both human and technical.  The issues of inclusion/exclusion and social access (or the lack thereof) are potential critical consequences of any health oriented network. Clients and health professionals alike could be disadvantaged if other modes of interaction are not available. “The information society might be conceptualized as a powerful technoeconomic network that is creating a new social reality. Drawing on the work of Latour, Star has described the way heterogeneous interests can be pulled together into 'mini-empires' enrolling both human and non-human actors into new techno-social networks. Once stabilized, these networks begin to shape our social landscape, grounding each and every social action and movement. Within these networks, new sets of physical-social conventions are established, which being stable for non-members, also creates new forms of marginality” (Page & Scott, 2001, p. 549).
The issues of inclusion/exclusion and social access (or the lack thereof) are potential critical consequences of any health oriented network. Clients and health professionals alike could be disadvantaged if other modes of interaction are not available. “The information society might be conceptualized as a powerful technoeconomic network that is creating a new social reality. Drawing on the work of Latour, Star has described the way heterogeneous interests can be pulled together into 'mini-empires' enrolling both human and non-human actors into new techno-social networks. Once stabilized, these networks begin to shape our social landscape, grounding each and every social action and movement. Within these networks, new sets of physical-social conventions are established, which being stable for non-members, also creates new forms of marginality” (Page & Scott, 2001, p. 549).